Poor data, or data poverty, is a formidable barrier for Health Information Exchanges (HIEs) and Health Information Networks (HINs) adapting to patient care in the digital age. In addition to HINs and HIEs of all sizes looking to reduce clinical risk, many hospitals and health systems are going through system changes and searching for a single solution data clean-up consultant to optimize care and operational efficiencies. In this blog, we’ll explore the overall economic impact of health data quality and why it’s so critical that companies implement a complete MPI solution.
What is health data quality?
Health data quality (HDQ) is how, where, and when healthcare data evolves over time, and whether it’s useful. Quality data is crucial to our entire healthcare system, especially as it rapidly becomes digitized, recorded, and stored electronically. Much of this health-related information is captured by patients themselves – and it’s amassing health data at extremely high rates. By making data more sophisticated and useful, HIE’s and HIN’s can discover better care coordination, greater clinical insights, and a healthier population.
The impact of health data poverty is only going to increase as more data-driven technologies become mainstream.
A barrier to equitable digital healthcare
We’ve said it many times – if you have bad data coming in, you’re going to have bad data going out. As a recent study describes, health data poverty is ‘the inability for individuals, groups, or populations to benefit from a discovery or innovation due to insufficient data that are adequately representative.’ That’s true – and it’s a real threat to current and future patient care.
Additionally, the quality of health data is crucial to organizational progress and revenue streams. Why? Because most revenue sources (Health Plans and Provider Organization Memberships) rely on this incoming health data to be timely and accurate to enhance patient safety, reduce re-admission rates, provide deeper insights into social determinants of health (SDOH), and improve operational efficiency.
Cost to Organizations: When poor quality data and patient duplication exists within hospitals and health systems, it reveals a compounding problem of operational and financial losses. In hospitals without effectively implemented EMPIs, rates of duplicate patient records can be very high. One Texas hospital found that duplicates accounted for 22% of all patient records. And costs resulting from inefficiencies associated with those duplicate records tallied $96 per duplicate. The burden of these duplicate patient records can be seen in the following areas:
- Patient registration
- Patient accounting
- Clinical errors
- Uninformed or unnecessary care
- Patient satisfaction
- Litigations
Consider an example from one of the areas above – patient accounting. Those staff members who handle insurance and billing must sort through disparate data compiled from different touchpoints within organizations (e.g., emergency department [ED], pharmacy, and admitting). They must work to discern what information goes with which records so they can send the right bills to the right patients or providers for the right amounts. This is not an automated, rules-based process but a manual process, prone to human error and oversight. It costs time and money to get it right. And getting it wrong could mean incorrect claim denials for patients, over-or-under billing, and additional operational insufficiencies.
For one client, 4medica removed over 800,000 duplicate health records in a system. That’s more than the entire population of Alaska.
Cost to Patients: In a hospital setting, a physician needs a patient’s ambulatory outpatient records to make evidence-based decisions about appropriate treatment. Too often, the data that would inform clinicians at the point of care are trapped in siloes scattered across the health care landscape. This means medical decisions are at serious risk if the wrong result is attached to the wrong patient. Patient safety issues arise when information is incorrect, and revenues are lost if the billing is inaccurate or order management is inefficient.
Incomplete information resulting from duplicate or partial records can contribute to clinical errors. For example, providers without access to single, complete patient records may be in the dark about the medications their patients are taking. This can lead to duplicate medications being prescribed as well as potential adverse events resulting from dangerous drug-to-drug interactions or drug allergies that may have been documented in one system but are missing from others.
The same can be seen in clinical areas where there is incomplete or disparate information. In a 2019 study, authors described a deep learning algorithm for predicting acute kidney injury in adults. Only 6.4% of the data in the training dataset was derived from female patients and the model was found to underperform in this group. This is a good example of gender-related health data disparities causing relative health data poverty in women.
Legal Impact
In many of these cases, hospitals will bear the cost of additional care to address these complications without additional revenue. Additionally, the cost of clinical errors can decrease revenue, patient satisfaction, employee and physician satisfaction, while steadily increasing privacy issues and litigation risks.
- A single litigation due to improper treatment can cost $500k
- Duplicate records can cost a single org up to $40M in total costs, according to AHIMA.org
The solution? Quality MPI data
Addressing poor patient data is key to solving clinical interoperability and profitability challenges. HIEs and HINs must take a 360 approach, but also must become patient-centric to process and communicate information. Value lies in providers’ ability to generate the quality of data, not quantity, to drive industry initiatives that accurately measure results and identify and improve gaps in the care continuum.
Reducing Duplicates with an EMPI: As with other forms of poverty, health data poverty is complex and not amenable to a single, simple solution. In choosing an EMPI solution, several factors must be considered. Look for a solution that can be scaled across your organization and offers the following elements:
- A single installer, ensuring you can start ingesting data quickly
- An approach to product design that allows the organization to move toward full independence quickly
- Easy-to-configure matching rules that enable you to monitor the health of the system
Once you’ve selected the best solution, work with your EMPI partner to decide which data sources to bring into the new system, assess the quality of that data, and start matching patient records to identify duplicates and gaps in information. Once the data is in the EMPI system, you will be able to focus on ongoing data stewardship, managing your duplicates going forward.
Achieving Heath Data Quality through technology
The Idaho Health Data Exchange incorporates advanced data sharing capabilities and actionable data insights. Learn how 4medica used technology to help them reduce duplication rates below 1% and deliver a longitudinal health record that stakeholders could trust to achieve optimal care management.
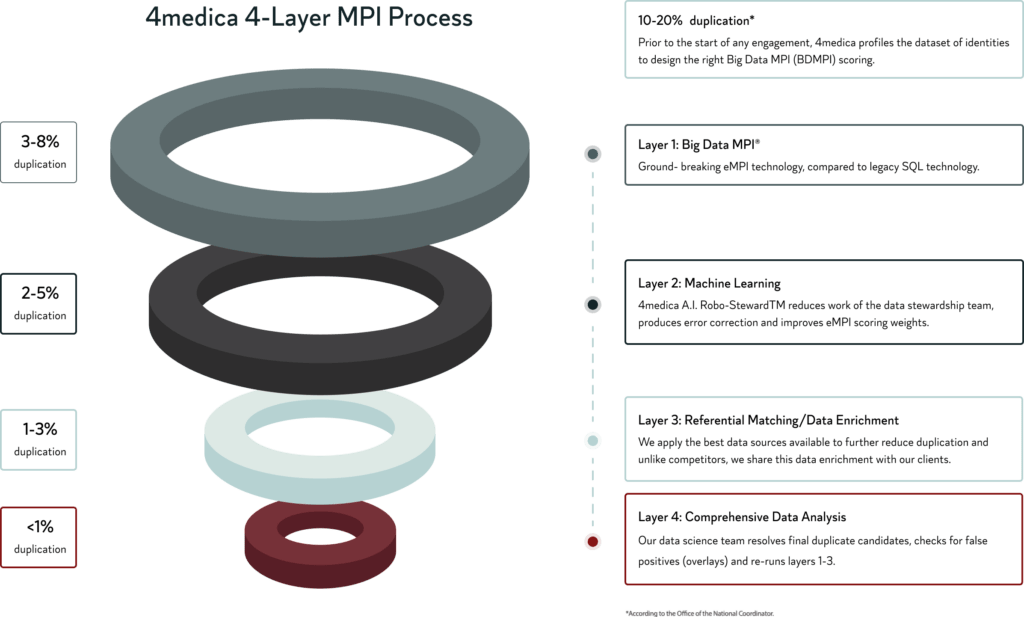
By utilizing the industry’s most technologically advanced MPI process, 4medica has revolutionized how HIEs & HINs can analyze and implement big data. Our 4-layer approach simplifies implementation and guarantees dramatic success of <1% patient duplication.
Good quality data is the foundation for accurate healthcare reporting and statistical analysis; it creates an atmosphere of trust where healthcare data is usable and provides value to participants and ultimately patients. It also allows for an effective revenue cycle management strategy, which can help reduce burnout.