Laboratory & Imaging Data Management
Low quality data = low revenue
- Significant loss of order-related revenue
- Lack of clinical interoperability impedes care coordination
- Inefficient RCM process
- Up to 30% payment denials
- Almost 20% losses in patient collections
Patient duplication and data-related errors can turn care coordination into a guessing game.
An opportunity for significant improvement
The lab and imaging market remains behind other healthcare sectors in recognizing the potential impact of quality health data on patient outcomes, operational process, and medical research. This is a huge missed opportunity.

A New Revenue Stream:
Optimized Outcomes:

Secure Systems:
Further Results of Poor Lab Data Management
When labs and imaging centers have inefficient processes they’re unable to provide significant quality assurance or guarantee accurate data transfer. Most lab processes used today are outdated legacy systems that can’t meet regulatory standards and lack the key features needed for proper lab operations and data storage.
Lab and imaging patients deserve better lab data management solutions. Practitioners and laboratories deserve simpler tools and efficient lab data management.
Interoperability of Laboratory Data
Lack of proper lab and imaging interoperability jeopardizes every aspect of lab function from sample management to patient reporting. In order for organizations to meet their legislative changes they need a top health data management and health data exchange platform. This system should provide the necessary technology and services to help labs achieve real-time interoperability success.
The 4medica Data Quality Platform
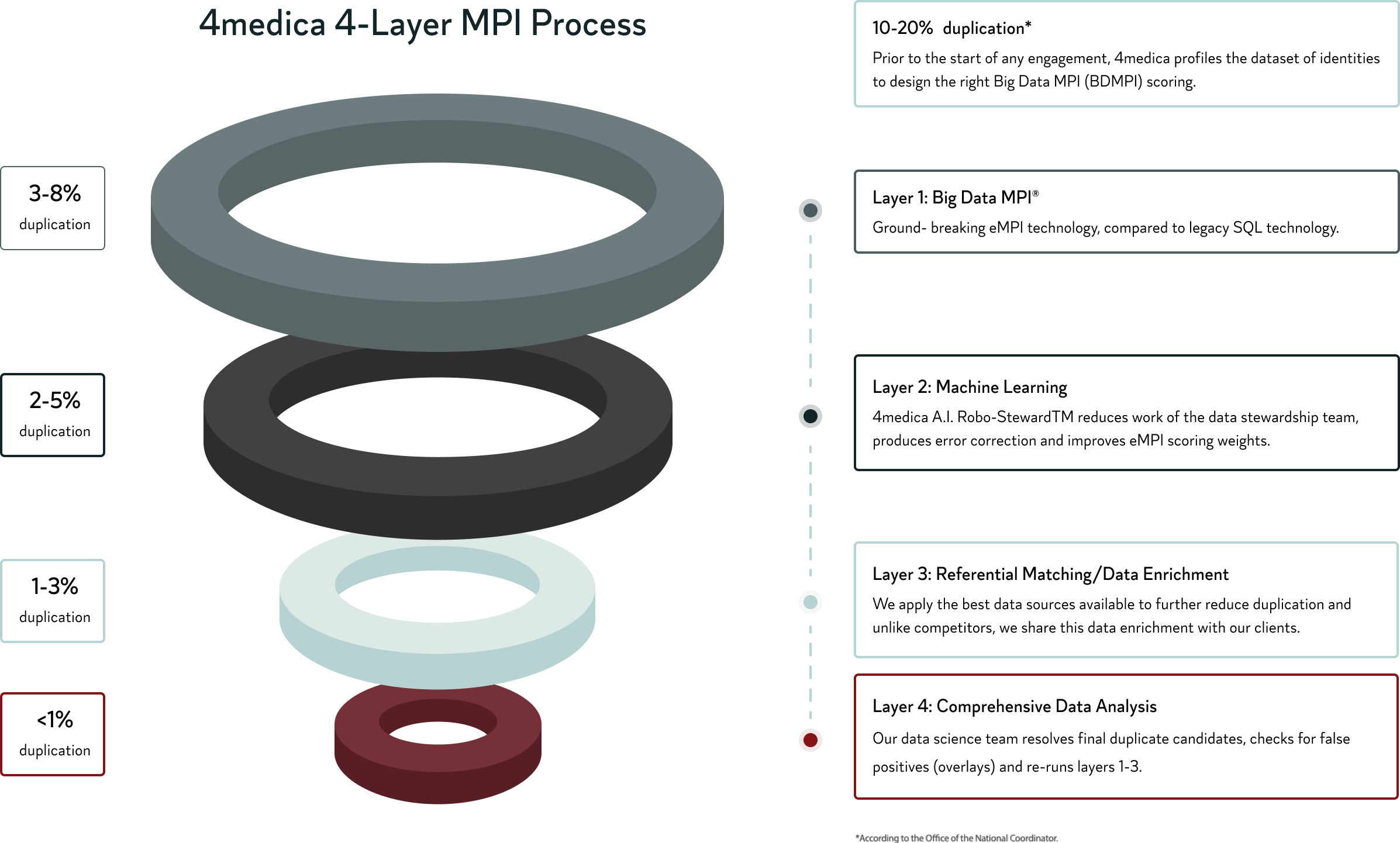
Utilizing the industry’s most technologically advanced MPI process, 4medica has revolutionized how Labs & Imaging Centers can analyze and implement big data. Our 4-layer approach simplifies implementation and guarantees dramatic success of <1% patient duplication.